Let me state the obvious: alcohol and marijuana are the two most widely used drugs of abuse in the United States. According to the annual National Survey on Drug Use and Health (NSDUH), (the most comprehensive survey of drug use and abuse in the United States conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA)) as of 2013, 86.8% of the population aged 18 or older have reported having consumed alcohol during their lifetime with over 16.6 million adults diagnosed with alcohol abuse disorder.
Of course, we all know the prevalence and extent of underage drinking, and the damage alcohol has on the developing brain has been heavily researched, not to mention all the significant secondary problems associated with alcohol abuse (car crashes, sexual assault on college campuses, falling off of balconies… ).
But here’s some numbers anyways: as of 2013, 8.7 million youths aged 12-20 reported past month alcohol use, a shockingly high number for an age group this is not legally allowed to drink alcohol…
Similarly, marijuana, which is still illegal in the vast majority of the US, is nearly as ubiquitous. According to the NSDUH 2013 survey, 19.8 million adults aged 18 or older reported past month marijuana use.
And with marijuana legalization in Colorado and Washington, a significant concern raised by many is that abuse of the drug among youths will dramatically increase even higher than it is now. The research supporting the damage marijuana can inflict on brain development is also significant.
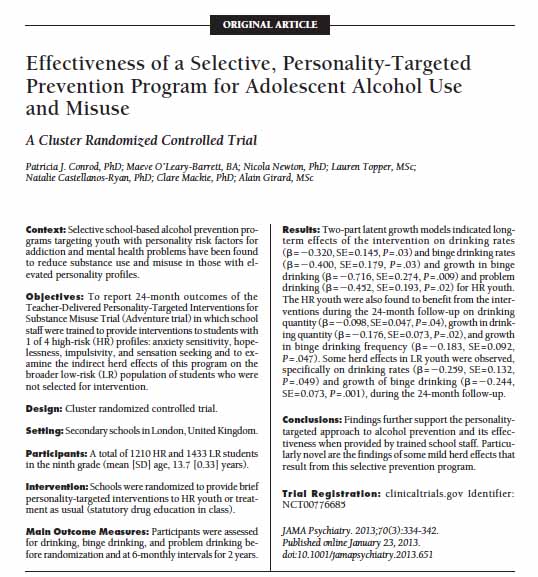
But what if the risk of use of alcohol and marijuana by youths could be reduced? What if a teacher could be given the tools to not only identify certain risky personality traits in their students but also use that knowledge to help those at-risk students from trying and using drugs such as alcohol and marijuana? A series of studies coming out of the laboratory of Dr. Patricia A Conrod of King’s College London report having done exactly that.
 I had the pleasure of seeing Dr. Conrod speak at the recent Society for Neuroscience Conference as part of a satellite meeting jointly organized by the National Institute on Drug Abuse (NIDA) and National Institute on Alcohol Abuse and Alcoholism (NIAAA). Dr. Conrod presented a compelling story spanning over a decade of her and her colleague’s work, in which certain personality traits amongst high risk youths, can actually be used to predict drug abuse amongst those kids. Dr. Conrod argues that by identifying different risk factors in different adolescents, a specific behavioral intervention can be designed to help reduce alcohol drinking and marijuana use in these youths. And who is best to administer such an intervention? Teachers and counselors, of course: educators that spend a great deal of time interacting with students and are in the best position to help them.
I had the pleasure of seeing Dr. Conrod speak at the recent Society for Neuroscience Conference as part of a satellite meeting jointly organized by the National Institute on Drug Abuse (NIDA) and National Institute on Alcohol Abuse and Alcoholism (NIAAA). Dr. Conrod presented a compelling story spanning over a decade of her and her colleague’s work, in which certain personality traits amongst high risk youths, can actually be used to predict drug abuse amongst those kids. Dr. Conrod argues that by identifying different risk factors in different adolescents, a specific behavioral intervention can be designed to help reduce alcohol drinking and marijuana use in these youths. And who is best to administer such an intervention? Teachers and counselors, of course: educators that spend a great deal of time interacting with students and are in the best position to help them.
The Teacher-Delivered Personality Targeted Interventions For Substance Misuse Trial, also known as the Adventure Trial, was conducted in London during 2008-2009 and the results were first published in 2010.
This ambitious study recruited 2,643 students (between 13 and 14 years old) from 21 secondary schools in London (20 of the 21 schools were state-funded schools). Importantly, this study was a cluster-randomized control trial, which means the schools were randomly assigned to two groups: one group received the intervention while the other did not. The researchers identified four personality traits in high-risk (HR) youths that increase the risk of engaging in substance abuse. The four traits are:
- Anxiety sensitivity,
- Hopelessness
- Impulsivity
- Sensation seeking.
A specific intervention based on cognitive behavioral therapy (CBT) and motivational enhancement therapy (MET) was developed to target each of these personality traits. Teacher, mentors, counselors, and educational specialists in each school that were recruited for the study were trained in the specific interventions. In general, CBT is an approach used in psychotherapy to change negative or harmful thoughts or the patient’s relationship to these thoughts, which in turn can change the patient’s behavior. CBT has been effective in a treating a number of mental disorders such anxiety, personality disorders, and depression. MET is an approach used to augment a patient’s motivation in achieving a goal and has mostly been employed in treating alcohol abuse.
The CBT and MET interventions in this study were designed to target one of the four personality traits (for example, anxiety reduction) and were administered in two 90-minute group sessions. The specific lesson plans for these interventions were not reported in the studies but included workbooks and such activities as goal-setting exercises and CBT therapies to help students to dissect their own personal experiences through identifying and dealing with negative/harmful thoughts and how those thoughts can result in negative behaviors. Interestingly, alcohol and drug use were only a minor focus of the interventions.
The success of the interventions was determined through self-reporting. The student’s completed the Reckless Behavior Questionnaire (RBQ), which is based on a six-point scale (“never” to “daily or almost daily”) to report substance use. Obviously due to the sensitive nature of these questionnaires and need for honesty by the students, measures were taken to ensure accuracy in the self-reporting, such as strong emphasis on the anonymity and confidentiality of the reports and inclusion of several “sham” items designed to gauge accuracy of reporting over time. Surveys were completed every 6-months for 24-months (two years) which is a sufficient time frame to assess the effect of the interventions.
Most importantly, schools were blinded to which group they were placed in and teachers and students not involved in the study were not aware of the trial occurring at the school. The students involved were unaware of the real purpose and scope of the study. These factors are important to consider because it held eliminate secondary effects and helps support the direct efficacy of the interventions themselves.
The results were impressive: reduced frequency and quantity of drinking occurred in the high-risk students that received the intervention compared to the control students that did not. While HR students were overall more likely to report drinking than low-risk (LR) students, the HR students saw a significant effect of the personality-targeted interventions on drinking behavior.
A study of this size is incredibly complex and the statistics involved are equally complex. The author’s analyzed the data in a number of ways and published the results in several papers. A recent study modeled the data over time (the 24-months in which the surveys were collected) and used these models to predict the odds that the students would engage in risky drinking behavior. The authors reported a 29% reduction in odds of frequency of drinking by HR students receiving the interventions and a 43% reduction in odds of binge drinking when compared to HR students not receiving the interventions.
Interestingly, the authors report a mild herd-effect in the LR students. Meaning that they believe the intervention slowed the onset of drinking in the LR students possibly due to the interactions between the HR student’s receiving the interventions and LR students. However, additional studies will need to be done in order to confirm this result.
Recall that the Reckless Behavior Questionnaire (RBQ) was utilized in this study to quantify drug-taking behavior. While the study was specifically designed to measure effects on alcohol, the RBQ also included questions about marijuana. So the authors reanalyzed their data and specifically looked at effects of the interventions on marijuana use.
The found that the sensation seeking personality sub-type of HR students that received an intervention had a 75% reduction in marijuana use compared to the sensation seeking HR students that did not receive the intervention. However, unlike the findings found on alcohol use, the study was not able to detect any effect on marijuana use for the HR students in general. Nevertheless, the data suggest that the teacher/counselor administered interventions are effective at reduce marijuana use as well.
While you may be unconvinced by the modest reduction in drinking and marijuana frequency reported in these studies and may be skeptical of the long-term effect on drug use in these kids, keep in mind that the teachers and counselors that administered these interventions received only 2 or 3 days of training and the interventions themselves were very brief, only two 90-minute sessions. What I find remarkable is that such a brief, targeted program can have ANY effects at all. And most importantly, the effects well outlasted the course of the interventions for the full two-years of the follow-up interviews.
These targeted interventions have four main advantages:
- Administered in a real-world setting by teachers and counselors
- Brief (only two 90-minute group sessions)
- Cheap (the cost of training and materials for the group sessions)
- Effective!
The scope of this intervention needs to be tested on a much larger cohort of students in a larger variety of neighborhoods but it is extremely promising nonetheless. Also, it would be interesting to breakdown these data by race, socioeconomic status, and gender, all of which may impact the effectiveness of the treatments and was not considered in this analysis. Finally, how would you implement these interventions on a wide scale? I eagerly look forward to additional work on these topics.
Thanks for reading 🙂
See these other articles in Time and on King’s College for less detailed discussions of these studies.
Also see these related studies from Conrod’s group: